By Jegason P. Diviant
Volume 6 Issue 1
Inflammation is an important part of our body’s innate immune response to harmful stimuli, such as irritants, toxins, cellular damage, and pathogens. It is often characterized by redness, heat, swelling, pain, and sometimes the loss of function. After the harmful stimuli have been removed, the healing process of the cells and tissues can begin. Acute inflammation is generally looked at as a first line of defense against a tissue injury or exposure to a pathogenic microbe. It involves very complex vascular and cellular components and responses. It has a rapid onset and usually lasts for a few days or weeks. Without inflammation, we would not be able to heal and recover.
Chronic inflammation is a prolonged inflammatory reaction. It’s often associated with the persistence of pathogenic microbes or foreign bodies, and sometimes it’s associated with autoimmune reactions. This type of inflammation most always results in cellular and tissue destruction. It can last for many months, years, or possibly life. Symptoms associated with chronic inflammation can include fatigue, pain, fever, rashes, and sores. Depending on the cells and tissues involved, it can also result in cognitive, behavioral, and mood disturbances. The onset is much slower than with acute inflammation. If the acute inflammatory pathways are unable to resolve the source of irritation and damage, or eliminate the pathogenic microbes, then chronic inflammation may set in. With autoimmune reactions, the immune system attacks normal, healthy tissue, mistaking it for a foreign body or pathogen. There’s a large body of evidence associating chronic inflammation with pathogenic microbes, toxins, heavy metals, dietary habits, nutritional deficiencies, and food sensitivities. In fact, just about all cognitive, behavioral, and mood dysfunctions can be associated with chronic inflammation.
An emerging field of research has been focusing on the bridging of neuroendocrine psychology and gastroenterology. While most of us are familiar with the central nervous system (CNS) and the peripheral nervous system (PNS), did you know that we have another nervous system consisting of more than 500 million neurons? This system is referred to as the enteric or intrinsic nervous system. It’s also known as the second brain. It’s capable of acting independently of the sympathetic (fight or flight) and parasympathetic (rest and digest) nervous systems, which are both part of the autonomic nervous system (ANS). The signaling that takes place between the gastrointestinal tract and the central nervous system is known as the gut-brain axis. This bidirectional, biochemical signaling network is further influenced by the microbes in our intestinal tract. We have a very special relationship with these microbes. We supply food for them and in return they synthesize water-soluble B vitamins, such as thiamine (B1), riboflavin (B2), pantothenic acid (B5), pyridoxine (B6), biotin (B7), folic acid (B9), and cobalamin (B12). They also synthesize a wide variety of organic acids and vitamin K. The microorganisms in our gut can have a profound effect upon neurotransmitter production and regulation. Some species of lactobacilli are able to produce or influence the release of both GABA and serotonin. Many members of the Bifidobacterium genera are able to influence GABA as well, which is extremely important because GABA is the chief inhibitory neurotransmitter of the body. Some bacillus species influence noradrenaline and dopamine, and Lactobacillus plantarum has been shown to influence acetylcholine, histamine, and serotonin production and regulation. This is just the tip of the iceberg in terms of what the microbes in our gut can do for us. They have a profound impact upon how our immune system functions, how we’re able to digest food, and there’s a tremendous amount of evidence associating dysbiosis (an impaired microbiota) with leaky gut syndrome, gastrointestinal inflammation, and autoimmunity.
It’s generally stated that bacterial cells in our body and on our body surfaces outnumber our own cells 10:1. This number doesn’t take into account the fungi, viruses and archaea, which also make up our microbiome, so the ratio is probably much higher in terms of microbial units to human cells. There are roughly 20,000 genes in the human body, but there are several millions of genes contained within the various members of the human microbiome. Anything that disrupts the microecology in our gut (dysbiosis) will affect neurotransmitter production, communication to and from the CNS, regulation of the sympathetic and parasympathetic nervous systems, hormone production, nutrient absorption and synthesis, and autoimmunity. We now know that a healthy gut microbiota is necessary for optimal physical and mental health.
Even pathogenic microorganisms such as Candida albicans, Escherichia coli and Clostridium difficile can be found residing within a healthy and functioning gut microbiota. Their presence alone does not indicate a disease state. When the ecology and population of these pathogens becomes abnormal and imbalanced, chronic inflammation and leaky gut can set in, leading to systemic infections, known as sepsis.
There are many pro-inflammatory and anti-inflammatory pathways in the body and many ways to modulate them. One way is through the body’s endocannabinoid system. But, what exactly is the endocannabinoid system? It’s rarely discussed in the college classroom setting, and this is true of both undergraduate and graduate-level curricula, such as medical school and pharmacy school.
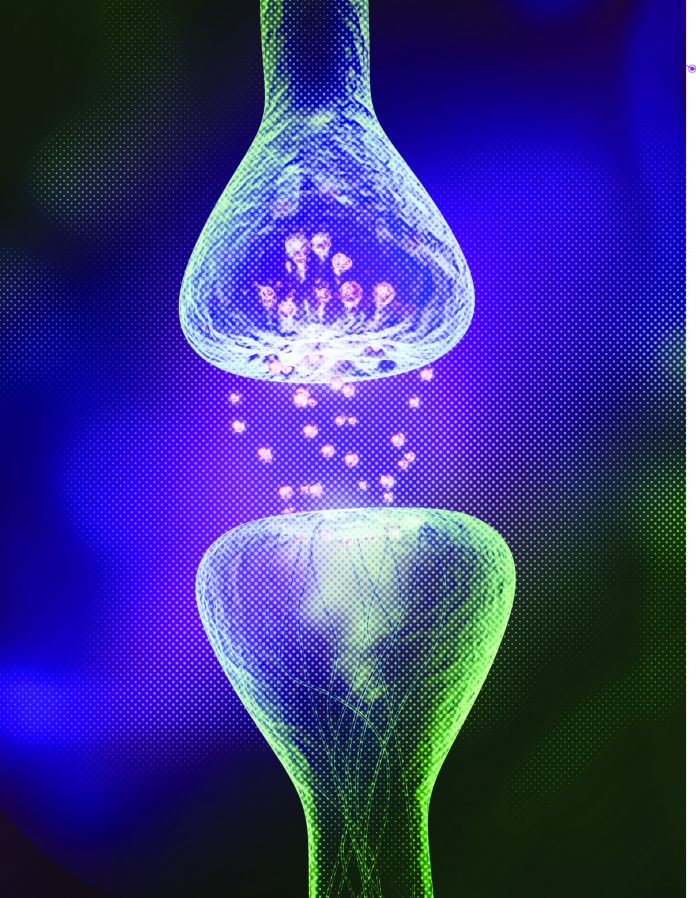
To begin with, there are two very well-known major receptors in the endocannabinoid system: CB1 and CB2. Both are known as G protein-coupled receptors (GPCRs). This is the largest known class of membrane receptors. They reside within the cellular membrane, and initiate signaling within the cell, influencing many different intracellular functions. Anandamide was the first endocannabinoid to be discovered, and is also known as N-arachidonoyl-ethanolamine or AEA. The second endocannabinoid to be discovered was 2-arachidonylglycerol or 2-AG. The discovery of the CB1 receptor was announced in 1990 and the CB2 receptors was credited as being discovered a few years later in 1993. Anandamide was discovered in 1992, and 2-AG was discovered in 1995. Since then, many other endocannabinoids have been discovered.
CB1 receptors are responsible for psychotropic effects in addition to the regulation of learning and memory, neuronal development and synaptic plasticity, neuroinflammation and degeneration, metabolism and food intake, bone mass, and pain reduction. It can be activated by both AEA and 2-AG, in addition to tetrahydrocannabinol (THC). CB2 receptors can be found all over the body, and are mostly activated by 2-AG. They’re widely abundant on immune cells. They’re found all throughout the gastrointestinal system. They are also be found on microglial cells in the brain, which are a primary component of active immune defense within the CNS. They’re found within the PNS in addition to many different organs, such as the liver, pancreas, spleen, thymus, and tonsils. The activation of CB2 receptors is likely a viable target for the treatment of allergies, autoimmune disorders, inflammation, neurodegenerative diseases, chronic pain, alcohol and nicotine addiction, as well as other diseases. In fact, there is a large body of peer-reviewed literature indicating that both the CB1 and CB2 receptors may be viable targets for the treatment of a wide variety of cancers. In addition to CB1 and CB2 receptors, endocannabinoids can activate many other GPCRs. Vanilloid, serotonin, glycine, NMDA, dopamine, orexin, acetylcholine, and others. CB1 receptors can form heterodimers with many of these receptor classes, and CB2 receptors can form heterodimers with chemokine receptors in both healthy tissue and cancerous cells. Exogenous cannabinoids, such as THC, CBD, CBN, CBC, CBG, and others, in addition to terpenes, terpenoids, flavonoids, and other molecules synergistically work together in modulating the endocannabinoid system, in what we often refer to as the entourage effect.
What are some chronic inflammatory disorders that can be treated with cannabis? The list is very extensive, but some well-known disorders include Crohn’s disease, inflammatory bowel disease (IBD), colitis, hepatitis, fibromyalgia, dermatitis, and arthritis. Autoimmune diseases that can be treated with cannabis include multiple sclerosis (MS), Hashimoto’s thyroiditis, type-1 diabetes, lupus erythematosus, and rheumatoid arthritis. Often, autoimmune disorders are also associated with chronic inflammation, and as we’ve learned, the endocannabinoid system may regulate both chronic inflammation and autoimmunity. Given that inflammation in the gut can be associated with inflammation throughout the body, in addition to the production of autoantibodies, it makes sense that by addressing inflammation in the gut a huge spectrum of disorders in the body can also be addressed. This is all just the tip of the iceberg in terms of describing what the endocannabinoid system is, what systems in the body it influences, and what diseases can be treated by its activation. In this regard, it would make sense that a deficiency of endocannabinoids can be involved in many disease states. This is being recognized in the medical literature as endocannabinoid deficiency.